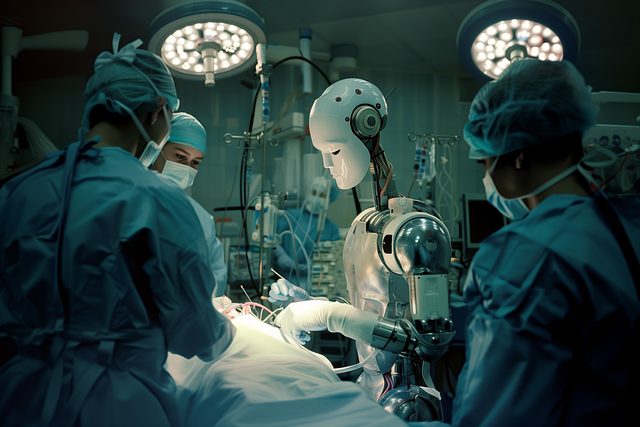
Regenerative care, led by innovative tissue repair therapy, is revolutionizing post-surgery recovery. This approach leverages the body's natural healing abilities to accelerate recovery, minimize scarring, and enhance overall well-being. By focusing on advanced cellular therapies, bioengineered scaffolds, and promoting angiogenesis, regenerative care improves surgical outcomes, reduces complications, and boosts patient satisfaction. Integrating complementary therapies like acupuncture, massage, and meditation further supports physical and mental resilience. Long-term benefits include reduced risk of chronic pain and scar tissue formation, enhancing quality of life and overall well-being.
In the pursuit of optimal post-surgical recovery, regenerative care emerges as a transformative approach, harnessing the body’s inherent healing capabilities. This comprehensive introduction delves into the multifaceted aspects of regenerative care, highlighting its potential to revolutionize patient outcomes. From understanding the science behind it to exploring innovative therapies like tissue repair, we navigate the path to faster healing, reduced scarring, and long-term prevention of complications.
- Understanding Regenerative Care: Unlocking the Body's Natural Healing Process
- The Role of Tissue Repair Therapy in Post-Surgical Recovery
- Comprehensive Approaches to Minimizing Scar Formation and Adhesions
- Integrating Complementary Therapies for Optimal Patient Comfort and Outcomes
- Long-Term Benefits: How Regenerative Care Can Prevent Future Complications
Understanding Regenerative Care: Unlocking the Body's Natural Healing Process

Regenerative care is a revolutionary approach that leverages the body’s inherent ability to heal itself, transforming traditional post-surgery recovery into an active process of tissue repair and regeneration. At its core, this concept focuses on stimulating and enhancing the natural healing mechanisms within the body, aiming to optimize recovery outcomes.
Understanding regenerative care involves recognizing the body as a sophisticated system capable of self-restoration. Through various therapeutic modalities, such as tissue repair therapy, this approach seeks to accelerate and support the body’s natural responses. By promoting the growth of new, healthy tissues while minimizing scar formation, regenerative care offers a promising path towards faster recovery, improved functionality, and enhanced overall well-being post-surgery.
The Role of Tissue Repair Therapy in Post-Surgical Recovery

Tissue repair therapy plays a pivotal role in enhancing post-surgical recovery, offering a holistic approach to healing. This innovative treatment focuses on stimulating and activating the body’s inherent regenerative capabilities, ensuring optimal tissue repair and restoration. By harnessing the body’s natural processes, tissue repair therapy accelerates the recovery timeline, reducing the risk of complications and improving overall patient outcomes.
The method employs various techniques, including advanced cellular therapies and bioengineered scaffolds, to create an environment conducive to tissue regeneration. These strategies promote the growth of new, healthy cells, replacing damaged or removed tissues, leading to faster healing and improved functional recovery. The integration of tissue repair therapy into post-surgical care routines is a game-changer, promising enhanced patient satisfaction and quicker returns to daily activities.
Comprehensive Approaches to Minimizing Scar Formation and Adhesions
Comprehensive approaches to minimizing scar formation and adhesions after surgery are crucial for optimal tissue repair and patient outcomes. One such approach involves the use of advanced tissue repair therapies, which go beyond traditional methods. These innovative treatments aim to stimulate the body’s natural healing processes by promoting angiogenesis—the growth of new blood vessels—and enhancing collagen production, both essential for robust tissue regeneration.
By incorporating these therapeutic interventions early in the recovery process, healthcare professionals can significantly reduce scar visibility and adhesion formation. This is particularly beneficial for surgeries involving large incisions or those at high risk for adhesions, such as abdominal procedures. The goal is to foster a healing environment that facilitates normal tissue architecture and function, ultimately improving patient comfort and aesthetic outcomes.
Integrating Complementary Therapies for Optimal Patient Comfort and Outcomes
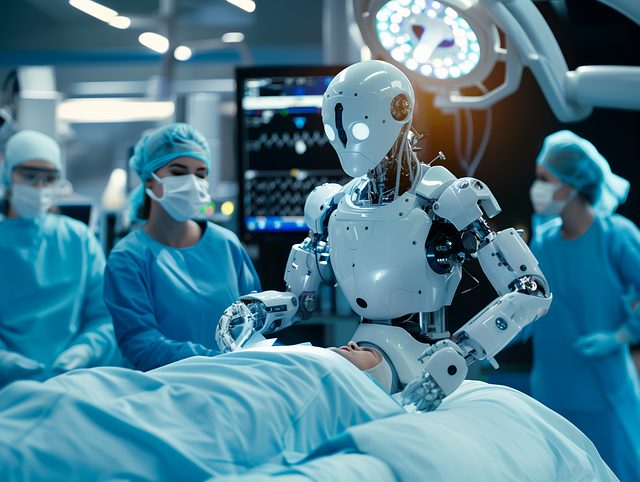
Integrating complementary therapies into post-surgical care regimens can significantly enhance patient comfort and improve overall outcomes, especially when focused on tissue repair therapy. These therapeutic approaches go beyond conventional medical treatments, offering a holistic perspective that addresses not just the physical wound but also the patient’s emotional and psychological well-being. Techniques such as acupuncture, massage therapy, and guided meditation can reduce pain, decrease anxiety, and speed up the healing process.
By incorporating these complementary practices, healthcare providers can create a more personalized and effective recovery plan. For instance, acupuncture has been shown to stimulate blood flow, promote tissue regeneration, and alleviate post-operative discomfort. Similarly, massage therapy improves circulation, reduces muscle tension, and enhances the body’s natural inflammatory response, all of which contribute to faster healing. Integrating these therapies ensures patients receive comprehensive care that supports not only their physical recovery but also their mental and emotional resilience during the regenerative process.
Long-Term Benefits: How Regenerative Care Can Prevent Future Complications

Regenerative care after surgery offers long-term benefits that extend far beyond immediate post-operative recovery. By harnessing the power of tissue repair therapy, patients can prevent future complications and enjoy improved overall health. This approach focuses on restoring and regenerating damaged tissues, promoting natural healing processes, and enhancing cellular regeneration. The result? A reduced risk of chronic pain, scar tissue formation, and other long-term issues commonly associated with traditional surgical recovery.
Through various techniques such as stem cell therapy, platelet-rich plasma (PRP), and bioregenerative matrices, regenerative care promotes the growth of new, healthy tissues. This proactive approach not only accelerates healing but also strengthens the body’s natural defenses against future injuries or conditions. By addressing underlying issues and fostering a robust healing environment, regenerative care ensures that patients are better equipped to handle challenges down the line, leading to improved quality of life and long-term well-being.
Comprehensive regenerative care, encompassing various therapeutic approaches like tissue repair therapy, represents a holistic evolution in post-surgical recovery. By harnessing the body’s inherent healing abilities and integrating complementary treatments, this care model significantly minimizes scar formation, enhances patient comfort, and prevents long-term complications. The evidence highlights its potential to revolutionize surgical aftercare, offering folks a more vibrant and active path to full recovery.
